What COVID-19 Does Inside the Human Body
COVID-19, caused by the novel coronavirus SARS-CoV-2, is far more than a typical respiratory illness—it is a relentless, stealthy invader capable of launching a full-scale attack on the human body. Since the virus first emerged, it has exposed deep vulnerabilities in our immune defenses, overwhelmed healthcare systems, and baffled even the most advanced scientific minds.
At first glance, COVID-19 may appear to be just another flu-like virus. Still, once it breaches the body’s defenses, it unleashes a sophisticated and often brutal assault on multiple organs and systems. It enters quietly, often undetected, exploiting the tiniest openings—the nose, mouth, or eyes—to begin its journey. However, once inside, COVID-19 rapidly takes over, hijacking cells and turning them into viral factories, producing millions of copies that spread like wildfire.
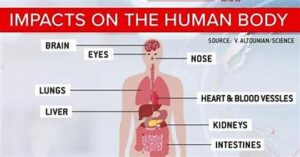
Its ability to mimic, mutate, and manipulate makes COVID-19 particularly treacherous. What begins in the lungs can cascade into a multi-organ crisis, affecting the heart, kidneys, brain, and more. The body, in turn, mounts a defense, but in doing so, sometimes causes as much harm as the virus itself. This internal war can range from mild symptoms to catastrophic failure, depending on how the body reacts to the invasion.
Understanding what COVID-19 does inside the human body is not just a matter of scientific curiosity—it is key to survival. With each wave, variant, and victim, we learn more about how this virus infiltrates, spreads, and lingers. It is a battle between an intelligent pathogen and the resilience of the human body. And as the virus continues to evolve, so too must our knowledge and defenses. This is the story of how COVID-19 challenges our biology, our medicine, and our humanity from the inside out.


Entry and Invasion: The Silent Intruder
COVID-19 does not announce its arrival with blaring symptoms—it slips into the body quietly, often undetected. The virus spreads primarily through respiratory droplets expelled when an infected person coughs, sneezes, speaks, or even breathes. These microscopic droplets can linger in the air or settle on surfaces, waiting for an unsuspecting host. When inhaled through the nose or mouth, or, in some cases, absorbed through the eyes, COVID-19 begins its covert invasion.
The virus’s first point of contact is typically the moist, mucosal lining of the respiratory tract. Here, it seeks out a very specific target: cells that display the ACE2 receptor on their surfaces. These receptors, which are naturally present in various tissues throughout the body, serve as a biological doorway. COVID-19’s infamous spike protein acts like a master key, binding to the ACE2 receptors with high precision. This interaction is what allows the virus to gain entry into the host cell—like a skilled thief unlocking a door.
Once inside, the virus doesn’t waste time. It hijacks the host cell’s internal machinery—specifically the ribosomes and enzymes—forcing them to stop normal functions and instead begin producing viral components. In a matter of hours, a single infected cell can be transformed into a factory churning out tens of thousands of viral copies, each equipped with its spike proteins and ready to spread.
These newly created virus particles burst out of the host cell, often destroying it in the process. They go on to infect surrounding cells, setting off a chain reaction of viral replication. What began as a small infiltration rapidly evolves into a widespread cellular takeover. The body’s tissues, especially in the nose, throat, and lungs, become the frontlines of an escalating conflict. With each replication cycle, the virus grows stronger in numbers, spreading deeper into the respiratory tract—and possibly beyond.
This early stage of infection is crucial. In many cases, individuals may feel no symptoms, making them unaware that COVID-19 is already multiplying within. During this time, the virus can be transmitted to others, fueling its spread throughout communities. The true danger of COVID-19 lies in this silent phase—when it quietly, efficiently, and ruthlessly prepares for a full-scale attack on the body.
Immune System Activation: The Body’s Counterstrike
The human immune system is a brilliant network of defenses designed to recognize, target, and eliminate foreign invaders. When functioning properly, it is swift, precise, and powerful. But COVID-19 is no ordinary enemy—it’s a master of disguise and delay. Unlike many viruses that trigger immediate immune reactions, COVID-19 has developed a way to delay detection, exploiting this critical window to spread deep into the body’s tissues before the alarm is raised.
When the immune system finally recognizes the threat, it activates with intensity. White blood cells—like neutrophils, macrophages, and T-cells—rush to the site of infection. These frontline warriors unleash a barrage of biochemical weapons: cytokines, interferons, and other inflammatory signals that help destroy infected cells and slow the virus’s spread.
In most cases, this immune response is sufficient to stop COVID-19. The virus is contained, and the body begins to recover. But in some individuals—particularly those with weakened or overreactive immune systems—this defense mechanism becomes dangerously unbalanced.
Instead of a targeted strike, the immune system launches an indiscriminate cytokine storm—an uncontrollable flood of inflammatory chemicals that can cause widespread collateral damage. Blood vessels leak, tissues swell, and organs begin to fail. The body’s own defenses, meant to protect, become a source of destruction. This hyperinflammatory response is one of the most lethal complications of severe COVID-19, often requiring intensive care and sometimes leading to multi-organ failure or death.

Lung Assault: The Primary Battleground
While COVID-19 can affect many parts of the body, the lungs are undeniably its most vicious battlefield. After entering through the upper airways and passing the body’s initial barriers, the virus descends into the lower respiratory tract, where it seeks out the delicate alveoli—tiny air sacs where oxygen and carbon dioxide are exchanged with each breath.
Inside the alveoli, COVID-19 goes on the offensive. It attacks the epithelial cells that form the thin walls of these air sacs, triggering inflammation and causing fluid to seep into the lung tissue. As the inflammation worsens, the lungs become stiff, heavy, and oxygen-starved. This condition—viral pneumonia—is a hallmark of moderate to severe COVID-19 cases.
For many patients, breathing becomes painful and labored. Oxygen levels in the blood plummet, leading to hypoxemia, which can affect every organ in the body. If the infection and inflammation continue to escalate, the patient may develop acute respiratory distress syndrome (ARDS)—a life-threatening condition where the lungs essentially shut down. At this stage, many require high-flow oxygen, non-invasive ventilation, or intubation with a mechanical ventilator to survive.
However, even if the body defeats the virus, the war may leave scars. Survivors of severe COVID-19 often experience long-term damage to lung tissue. Fibrosis, or scarring of the lungs, can lead to lasting breathing problems, reduced physical endurance, and chronic cough. For some, the respiratory system never fully returns to its pre-infection state—highlighting the long shadow COVID-19 can cast on a survivor’s life.
Beyond the Lungs: A Body Under Siege
While COVID-19 is widely known as a respiratory illness, its destructive reach extends far beyond the lungs. Once it establishes itself in the body, COVID-19 becomes a systemic predator, capable of disrupting the functions of nearly every major organ. Its impact is often multifaceted, unpredictable, and devastating, transforming a viral infection into a full-body health crisis.
The Heart Under Attack
COVID-19 has a profound effect on the cardiovascular system. The virus can trigger myocarditis, an inflammation of the heart muscle, which weakens the heart’s ability to pump blood and can lead to heart failure. Many patients also develop arrhythmias—dangerously irregular heartbeats—that can be fatal if left untreated. Even those with no prior heart conditions may experience lingering cardiovascular issues post-infection. In severe cases, the combination of viral inflammation and oxygen deprivation can lead to cardiac arrest.
Kidneys in Crisis
The kidneys, critical for filtering waste and regulating fluid balance, are also vulnerable. COVID-19 can directly infect kidney tissues or damage them indirectly through inflammation and clotting disorders. Many hospitalized patients suffer from acute kidney injury, with some requiring dialysis to survive. These kidney complications can linger long after the virus is cleared, raising the risk of chronic kidney disease.
Liver Complications
Though not a primary target, the liver often bears the brunt of the systemic inflammation COVID-19 causes. Elevated liver enzymes are frequently observed in blood tests, indicating liver stress or damage. In patients with pre-existing liver conditions, such as hepatitis or fatty liver disease, COVID-19 can worsen the condition, complicating recovery and increasing mortality risk.
Deadly Blood Clots
Perhaps one of the most sinister aspects of COVID-19 is its ability to cause hypercoagulability—an increased tendency for the blood to clot. These abnormal clots can lead to pulmonary embolisms, deep vein thrombosis, heart attacks, or strokes, sometimes with little warning. These complications can occur even in young, otherwise healthy individuals, making them some of the most alarming aspects of COVID-19’s systemic threat.
Neurological Havoc
COVID-19’s impact on the nervous system is equally concerning. Many patients experience headaches, dizziness, brain fog, and seizures, even weeks after recovering from the initial infection. The virus can breach the blood-brain barrier, potentially causing encephalitis (brain inflammation), confusion, and delirium, particularly in older or critically ill patients. In extreme cases, it has been linked to strokes and long-term cognitive dysfunction.
Loss of Senses
Among the more peculiar and widely reported symptoms is the loss of smell (anosmia) and taste (ageusia). While often considered mild, this sensory deprivation can persist for weeks or even months, significantly affecting a person’s quality of life. These symptoms indicate that COVID-19 has a direct impact on the olfactory nerves and possibly even the brain itself.

COVID-19 is, without a doubt, a multisystem invader. Its ability to infiltrate so many areas of the body, from the heart and kidneys to the brain and blood vessels, makes it one of the most complex and formidable viruses in recent history. This isn’t just a disease of the lungs—it’s a biological siege that overwhelms the body’s defenses at every level, leaving behind both visible and invisible scars.
Long COVID: A Lingering Nightmare
Even after the initial infection clears, many people continue to suffer for weeks or months. This post-viral syndrome, known as Long COVID, includes symptoms such as chronic fatigue, joint pain, difficulty concentrating (also called “brain fog”), heart palpitations, and shortness of breath. Long COVID affects people of all ages—even those who experienced only mild initial symptoms. Researchers are still trying to understand its cause, but one thing is clear: COVID-19’s impact can persist long after the virus itself is gone.

Who’s at Risk? Vulnerability in Every Corner
While COVID-19 can infect anyone, its deadliest consequences are often seen in the elderly and individuals with chronic health conditions like diabetes, hypertension, obesity, or compromised immunity. However, the virus does not spare the young and healthy—many have experienced severe symptoms, hospitalizations, or long-term effects. The unpredictable nature of COVID-19 is one of the factors that make it so frightening.
Variants and Viral Evolution
COVID-19 is a mutating adversary. New variants emerge regularly—each with unique features that may make it more contagious, harder to detect, or resistant to previous immunity. Variants such as Delta and Omicron have changed the landscape of the pandemic, causing new waves of infection. This evolution underscores the importance of continuous surveillance, updated vaccines, and robust public health responses. As long as COVID-19 is spreading, it will continue to evolve.
Vaccines: The Shield of Science
Vaccines have become our most powerful tool in the fight against COVID-19. By exposing the body to a harmless part of the virus—such as the spike protein—they teach the immune system how to recognize and destroy COVID-19 before it can take hold. Though not always perfect in preventing infection, vaccines drastically reduce the risk of severe illness, hospitalization, and death. Booster doses further reinforce immunity, especially in the face of evolving variants. Widespread vaccination is critical to slowing the spread and ending the pandemic.

The Global Impact: A Crisis Beyond Health
COVID-19 has affected every corner of the globe, disrupting lives, economies, and mental health. Lockdowns, job losses, overwhelmed hospitals, and isolation have taken a toll on societies worldwide. Yet amid the devastation, COVID-19 has also sparked unprecedented global collaboration. Scientists, governments, and citizens have united in their efforts to combat the virus with innovation, empathy, and perseverance.
Conclusion: Resilience Against a Ruthless Foe
COVID-19 is more than just a disease—it is a global reckoning. It has tested the limits of our medical systems, challenged our mental and physical strength, and reshaped how we live and connect. As we battle this ever-changing virus, one truth stands clear: knowledge, vigilance, and compassion are our strongest weapons. By understanding what COVID-19 does inside the human body, we are better equipped to fight it—together.
Explore more about What COVID-19 Does Inside the Human Body and understand India’s economic and human Losses Due to Coronavirus in detail.





















Recent Comments